Road to Recovery
At Kendall County Women’s Shelter, we often discuss how difficult it is for survivors to break free from the cycle of abuse. However, domestic abuse is only one of many battles our clients often face on their healing journey.
While most people do not initially link family violence with substance abuse issues, we know from our advocacy work and research efforts that these two issues are deeply intertwined.
For many, September represents National Recovery Awareness Month. Therefore, KCWS is sharing what we know about recovery from addiction, mental health issues, and abuse - and why these are all strongly related.
Evidence suggests that survivors of domestic abuse are more likely to misuse substances compared to those who have not endured abusive partners. In fact, in one study, half of women seeking housing services from domestic abuse agencies met criteria for substance abuse disorder (SUD; Poole et al., 2008).
Substance abuse disorder (SUD) is a diagnosable condition that follows the prolonged misuse of substances that have a significant effect on our health and ability to function in our daily lives (Cambell, 2002; McLellan. 2017). While alcohol is the most commonly abused substance amongst the general population, as well as amongst survivors of domestic abuse (Finney, 2004; Kraanen et al., 2014), addiction to illicit opioids, benzodiazepines, and cannabis are also common.
Individuals with SUD often become increasingly preoccupied with obtaining the substance they’ve developed an addicted to, consuming larger amounts than necessary to feel “buzzed” or “high.” This is usually followed by a state of unpleasant tolerance withdrawal symptoms, including agitation and anxiety. This discomfort often sparks a new search for substances.
The consequences of SUD, in most cases, are a typically a really poor mood and isolation from the social, occupational, or recreational activities an individual once valued.
Reality Check: It is important to understand that while survivors of domestic violence may be at an increased risk for SUD given their experiences, domestic abuse is not caused by substance abuse, nor is it a direct symptom of domestic abuse.
“He was [using] around me, and then he told me, ‘Just try it.’ So then I tried it. Then I got tangled into that, and I couldn’t get out of that relationship.”
Experts investigating the relationship between SUD and intimate partner violence have found that abuse is rooted in an perpetrators need for power and control over their partner. Survivors with SUD often believe that they are being abused because of their substance misuse, and feel that the agencies in place to support them will think the same.
But there is always a motivator behind a person’s behavior, and engaging in substance misuse is no exception.
For some survivors with SUD, their addiction was developed over time through acts of coercion from their abuser, where the survivor was forced to take substances.
In other cases, survivors feel that the repetitive abuse is too much of a burden to bear, and using substances is the only way to temporarily escape emotional and physical pain.
Regardless of what cultivated a survivor’s dependency on a particular substance, their is never justification for a perpetrator’s abusive actions.
What are Signs of Substance Abuse Disorder?
SUD is a serious health condition, and can contribute to poor psychosocial functioning, poor general physical health, and increased mortality. In fact, for those who do not meet the clinical diagnostic criteria for SUD, engaging in “risky levels of substance misuse” has also been linked to these adverse outcomes.
If believe that you or someone you know is suffering from addiction, there are signs to look out for:
Needing to use the substance regularly (in some cases, up to multiple times a day).
Intense cravings for the substance.
Needing more of the substance over time to produce the same “buzz” or “high.”
Taking more of the substance than intended.
Maintaining a supply of the substance at all times.
Spending resources obtaining the substance (time, money), even when those resources are limited.
Failing to meet responsibilities (school, work, etc.).
Driving under the influence.
Engaging in risky behaviors to obtain the substance (stealing, sexual acts, etc.).
Having multiple health issues.
Drastic and unpredictable behavioral changes.
Financial strain.
(Mayo Clinic, 2022)
“If we put out this message that alcohol … either directly or indirectly causes domestic violence, what we are saying to the survivors that are hearing that message is ‘If you can get your partner to sober up, then it’ll be better. And that is a really dangerous message.”
The Chicken and Egg Dilemma
We’ve noted that abuse is never acceptable, even if the partner is intoxicated and/or behaving in ways they normally would not.
But a commonly perpetuated stigma against survivors of domestic abuse with SUD remains that their addiction led to behaviors that resulted in their perpetrators abusive actions (“She was drunk and acting ridiculous. No wonder he reacted by screaming at her.”) But since many people use substances and do not abuse their partners, there must be other factors influencing these behaviors.
Reality Check: There seems to be a correlation between substance abuse and domestic abuse. But while substance abuse may increase the likelihood of abusive behavior, it does not cause or excuse it.
Researchers have noted the relationship between trauma exposure and substance abuse issues does seem to be cyclical. When posttraumatic stress symptoms increase, SUD symptoms seem to also elevate, and vice-versa.
So how do we explain the relationship between trauma exposure, such as domestic abuse, and SUD? Which really comes first?
The temporal relationship between domestic abuse and SUD is hard to tease apart, mostly because, posttraumatic stress symptoms and SUD often occur concurrently (Simonelli et al., 2014).
However, advanced research efforts using data obtained from survivors over time and meta-analytic techniques have suggested that domestic abuse more often precedes the onset of SUD (Øverup et al., 2015, Patrick et al., 2021), especially in the 1-2 years following the start of the abuse.
While these research efforts are a step in the right direction, additional studies are needed to truly understand what factors play a role in perpetuating or ending the cycles of abuse and addiction concurrently.
What We Think is Going On
There are two main theoretical frameworks that KCWS adopts to better understand our clients’ struggling with substance abuse. These are best illustrated by Strain Theory and Power Theory.
Numbing the Pain
Strain Theory, originally developed in the 1930s by American sociologist Robert K. Merton, has been used mostly in the context of explaining delinquent or criminal behavior. However, experts have recently began using this framework to explain the strong association between posttraumatic stress and SUD.
Strain theory posits that people may misuse substances in an attempt to cope with the overwhelming stress of their experiences.
At KCWS we’ve seen that isolation and gaining significant influence over a partner’s daily life/activities are some of the key tactics survivors report their abuser using to maintain a sense of power over them. According to Strain Theory, when traumatic domestic abuse, social isolation and a failure to meet personal goals co-occur, there may be an increase in risk for substance abuse.
The U.S. Department of Veterans Affairs and the U.S. Department of Defense (VA and DOD, respectively) have heavily invested in investigating the impacts of trauma exposure on the onset and maintenance of SUD in U.S. Military members, although these are often assessed in the context of combat-related trauma(s). However, these efforts have identified that in military populations, coping with posttraumatic stress symptoms via substance abuse is a common issue. While there is not quite as much literature readily available on the role of posttraumatic stress on the relationship between domestic abuse experiences and SUD, there are some things we do know:
Across studies, 60%–90% of survivors of domestic abuse meet diagnostic criteria for clinical PTSD (Golding, 1999; Dutton et al., 2005, 2006; Woods et al., 2008; Nathanson et al., 2012).
Additionally, survivors show greater PTSD symptom severity than trauma-exposed women who have not experienced domestic abuse (e.g. car accidents, natural disasters; Pico-Alfonso, 2005; Sullivan and Holt, 2008; Woods et al., 2008).
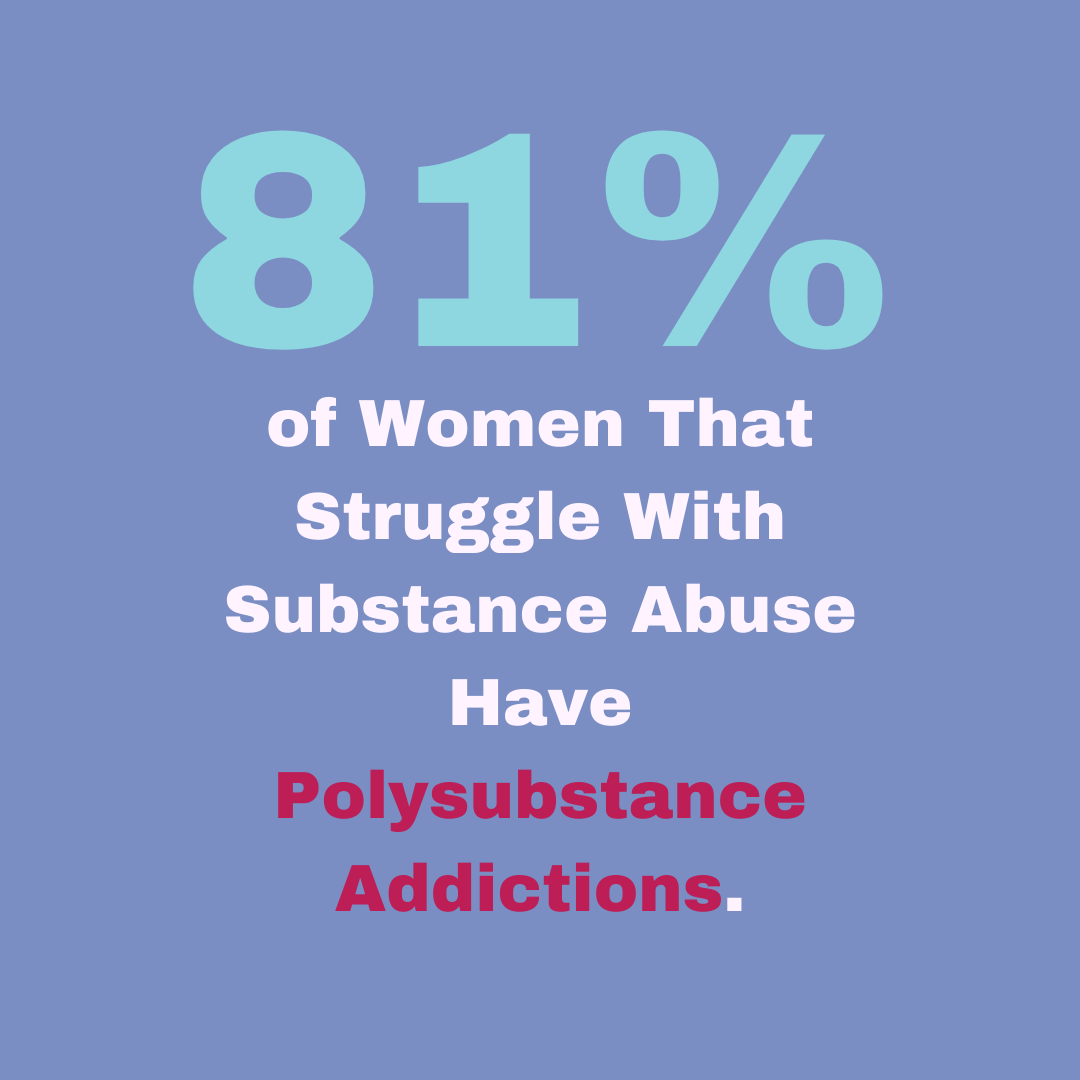
Further - Nearly half of women who develop PTSD due to domestic abuse develop comorbid SUD (Najavits and Hien, 2013).
Childhood trauma, social support, socioeconomic status, and a history of brain injury (which is also common in both domestic abuse and military populations) are all factors that seem to impact the relationships between domestic abuse and PTSD, as well as between PTSD and SUD (Baxter & Hellewell, 2019; Iverson et al., 2017; Jones et al., 2001; Salter & Breckenridge, 2014; Stalans & Ritchie, 2008; Vogel & Marshall, 2001).
While the U.S. military has made substance abuse issues a priority in service member healthcare, it is time we also heavily invest in understanding the role of PTSD in survivors of domestic abuse struggling with SUD.
2. Power & Control
If you follow KCWS, you know that we often emphasize the fact that an abuser’s actions are almost always motivated by a need for power and control over the survivor. Substances are often used as a tool for a perpetrator to obtain that power and control.
While it may be obvious that being forced to take substances would alter a person’s physical state, leaving them less likely to fight back against the abuse, the impacts of this coercion often go much deeper.
Abusers may use substances to alter consciousness in an attempt to limit survivors’ ability to call the police for help. If they do attempt to call law enforcement, the abuser may threaten to report survivors’ substance use.
Abusers may also threaten the survivors’ custody of their children because of their addiction, which the perpetrator often orchestrates to begin with.
Additionally, they may leverage stigma associated with substance use to isolate survivors from social networks and support systems.
And while it may seem far-fetched, abusers often use the survivor’s addiction to manipulate and mobilize institutional support systems (e.g., child welfare, criminal justice) against them.
Given these, power theory may also help explain the cyclic connection between domestic abuse and SUD, as abusers will often use both as tactics for power and control over another person.
“There are people who abuse alcohol, people who abuse drugs and don’t abuse their partners... [Abuser’s may think], If I medicate my partner, then she will be easier to handle. If I medicate my partner, she will fight less.”
So What Can We do to Help?
By educating yourself on the origins and impacts of addiction, particularly within survivors of domestic abuse, you have already taken the first step in making a difference for those choosing a life free from abuse. But there is always more to be done as advocates, practitioners, policy-makers, and researchers.
For individuals who do not work in social work or clinical settings, when aiding a survivor with SUD (such as a friend or family member), first ensure that you are coming from a place of support, and not judgement.
Reality Check: While you may know and love a person, you truly will never understand the feelings and experiences that resulted in their addiction.
Detox is usually an essential first part of the process of caring for a survivor with SUD. But additional support is often needed, such as continued in- or out-patient treatment, counseling or therapy to address both the abuse and addiction, as well as a potential need for appropriate medications at the right dosages (only if prescribed by a doctor).
If an individual is a domestic abuse survivor and struggling with SUD, it is critical they receive support for both issues.
Be patient with the survivor, and recognize if/when you should seek additional SUD resources for help that is outside of your capacity. Consider seeking your own form of emotional support if you become overwhelm with assisting a survivor in their healing journey.
As Agencies:
As either domestic abuse or substance abuse support centers, there are important steps we can take to better care for survivors with addiction issues:
Make safety as well as sobriety a top priority. Often a domestic abuse survivor’s partner is also using, and if they leave to find a more sober support network, there is increased risk to her safety. The most dangerous time for survivor is when they leave their abusers.
Recognize that even though the relationship may be a trigger for continued use, it may also be unsafe for them to leave. Survivors of domestic abuse often choose to stay with an abuser out of fear of further/lethal harm. Some survivors never leave their abuser for this reason.
Counselors should take into account the abuser's ability to sabotage substance abuse treatment through threats or fear.
Avoid language that implies the survivor caused their own abuse. Examples of words to avoid: codependency, enabling, and powerlessness. These do not hold the abuser fully accountable for his behavior.
Consider gender-specific treatment and support groups. Mixed groups may involve descriptions of male aggression directed toward female partners.
Provide access to childcare while they seek treatment.
Staff should be trained to understand and facilitate expressions of anger. This is often a sign of healing for survivors, and staff should be skilled to balance a survivor's need to release anger with the needs of others.
Counselors may need to address domestic abuse and SUD with different, but coordinated, interventions. Co-located services and SUD treatment, which includes education about domestic abuse co-facilitated by a domestic abuse advocate, have been shown to be particularly effective.
Keep an overdose kit on site, including Naloxone (a medicine that rapidly reverses an opioid overdose).
While the stages of change have been studied in women with both domestic abuse and SUD histories, practitioners should acknowledge that motivation toward change does not always ensure safety. This is because the abuser is the one who engages in the violent behavior. Safety-planning, or creating a formal plan for ensuring danger is minimized or eliminated in the future, with agency staff is particularly necessary in these cases.
“In certain situations, adult survivors of domestic violence may also have substance abuse issues. Substance abuse issues may have existed before the adult survivor’s abusive relationship. For other adult
survivors, the substance abuse may have come about as a direct result of being abused and traumatized in the current relationship. In order to engage in both trauma and domestic violence-informed practice, it is important to explore what the relationship is between the person using violence/coercive control and the adult survivor’s substance abuse. ”
KCWS strongly relies on community partnerships to meet the individual needs of our clients, who all come to us with their own unique histories and experiences. We often refer clients to seek additional care for SUD within local substance abuse centers. However, the development of integrated PTSD-SUD treatment options is a relatively new concept. Integrated therapies address more than one condition within one approach by prioritizing stabilizing the patient, teaching coping skills, and reducing the most destructive symptoms. Rather than diving deep into their traumatic experiences, integrated treatments first seek to establish the patient’s safety and well-being.
Given that the pathways leading to PTSD and SUD are neurobiologically and psychologically similar (Jacobsen et al., 2001), an integrated approach may be the most promising investment in trying to untangle the complexities of both abuse and addiction.
Read more about integrated PTSD-SUD treatment options here.
As Stakeholders, Policy-Makers, and Researchers
At KCWS, we know that SUD and additional mental health issues, such as posttraumatic stress, are consistent needs our clients seek services for. Trauma inevitably impacts one’s ability to function, which may lead to misusing substances as a coping strategy. In many cases, survivors begin to prioritize these substances over their safety.
We need to better understand the factors working as barriers to survivor care. By doing so,. we can increase SUD treatment availability and improve clinical outcomes for survivors. The big questions we should focus on are “Who is receiving care, and who are we missing?” , as well as, “Who gets better in treatment, and why?”
“In order for services to be effective, safe, and accessible to survivors, practitioners and policy makers need to understand the ways that substance use coercion impacts survivors and their children.”
Policy surrounding alcohol and other drug use should also reflect the realities of domestic abuse and its relationship to substance abuse. Mixed-messaging around these subjects often limits the protection of survivors and children from the issues, nor does it promote the prevention of future harm.
Other considerations for policy that take into account the impacts of both domestic abuse and SUD may include:
Promoting education and training on substance use coercion across systems that survivors and their children may use.
Improve community-level partnerships between domestic abuse and SUD treatment agencies.
Better equip services providers and systems to support survivors experiencing substance use coercion.
Strengthen survivors’ financial stability.
Encourage and invest in research on substance use coercion.
Cultivate a culture that values and seeks to deeply understand the barriers, progress, healing, and resiliency of persons with lived experiences as critical to informing all aspects of policy and practice.
KCWS is dedicated to providing comprehensive support, resources, and shelter for survivors and their pets, while also raising awareness about domestic abuse. As a support agency, we understand that we do not always have the capacity to manage a particular case on our own.
This is when we turn to other local agencies to fill any voids in services our clients may need, just as other agencies often seek our guidance in navigating domestic abuse issues for their own clients.
To untangle the complexities associated with both domestic abuse and SUD, as well as further promote together healthy family dynamics within our communities, treatment centers and domestic abuse support agencies should prioritize partnerships that lead to integrated strategies for care. By doing so, we can work smarter, not harder, in supporting those who have bravely made the choice to leave an abuser and heal from the chains of addiction.
If you, or someone you know, is struggling with substance abuse while also caught in the cycle of domestic abuse, help is available.
Call Kendall County Women’s Shelter today to create a safety-plan with our staff, and discuss options for addiction treatment.
KCWS 24/7 Hotline: 800-495-8078
About the Author
Prior to her service at KCWS as the Research & Education Coordinator, Sarah received a bachelor’s degree from the University of Colorado Boulder and a master’s degree in Psychology from the University of Texas at San Antonio. Having dedicated the past six years to researching factors related to posttraumatic stress, Sarah has collaborated with domestic abuse, foster care, and military support agencies. She is passionate about enhancing trauma-informed policies and practices, and is on track to obtain her PhD, Spring 2025.
Email: sarah@kcwstexas.org
KCWS Phone: 830.428.4930
Additional Resources:
CDC Resources for SUD:
International Overdose Awareness Day Toolkit
Linking People with Opioid Use Disorder to Medication Treatment
Understanding Addiction to Support Recovery
Recovery is Possible: Know the Options
Treatment of Opioid Use Disorder
Other:
Supporting Families Affected by Substance Use and Domestic Violence
KSAT News Article: Connection Between Domestic Violence and Substance Use